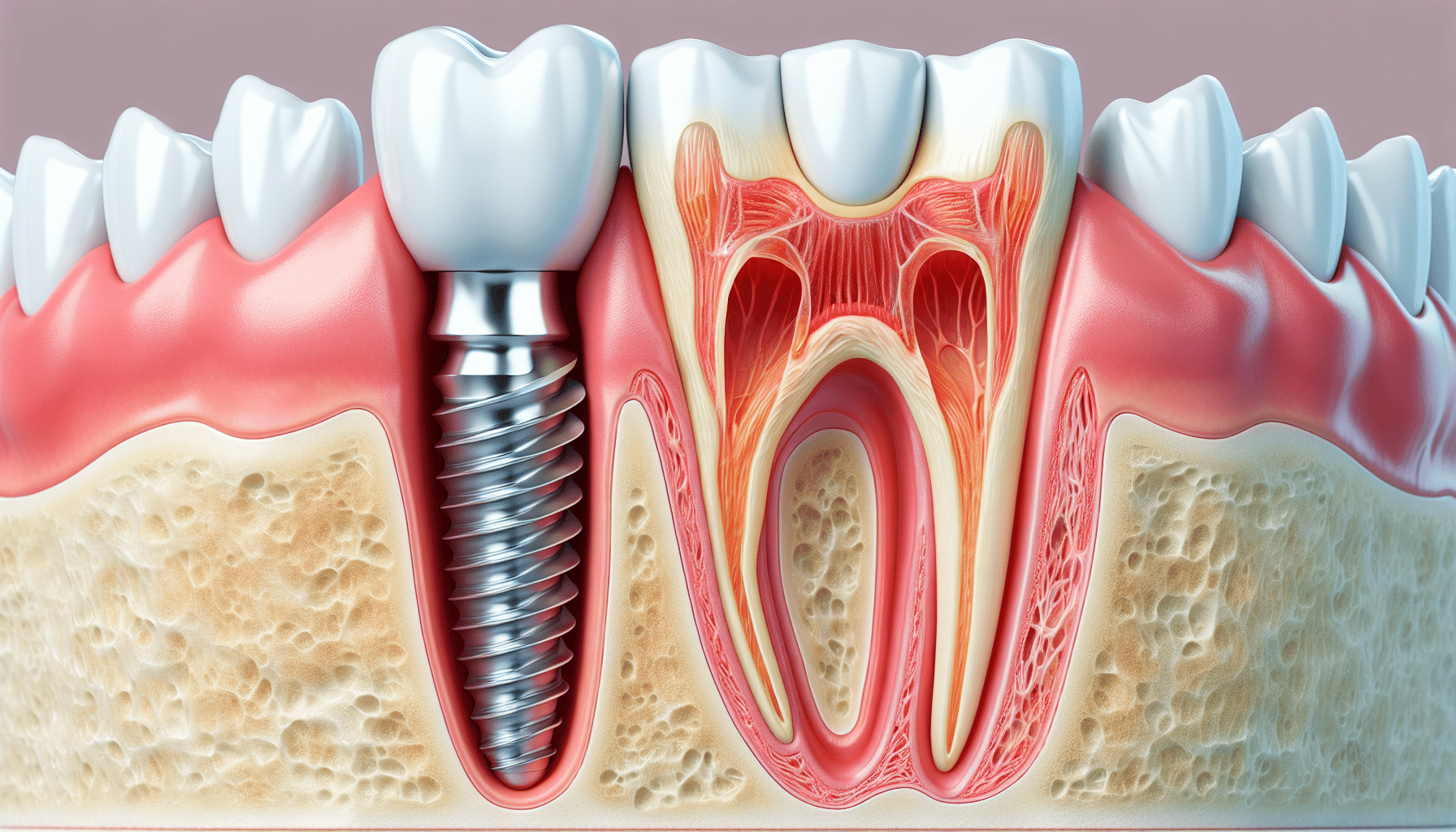
While dental implants demonstrate high success rates (95-97%), potential complications do exist. The most significant dental implant risks include peri-implantitis (occurring in 10-20% of long-term cases), osseointegration failure (1-2% of cases), and damage to adjacent anatomical structures, such as the inferior alveolar nerve or maxillary sinus. Research indicates smoking triples implant failure risk, while uncontrolled diabetes may reduce success rates by 30%.
Managing dental implant risks requires a comprehensive pre-treatment evaluation, including 3D CT scans, management of systemic diseases, and meticulous treatment planning. Precise surgical techniques with minimal bone manipulation, high-quality implants, and strict sterilization protocols further enhance outcomes. Postoperative compliance is equally critical – patients must maintain meticulous oral hygiene, avoid smoking, and attend biannual check-ups. Any warning signs, like persistent pain, implant mobility, or progressive swelling, warrant immediate dental consultation to prevent complications from escalating. These preventive measures collectively optimize implant longevity and functionality.
Let’s explore dental implant risks and complications together, understanding the risks, how to address them if they occur, and, most importantly, how to prevent them.
Common Dental Implant Risks and Side Effects
At D’Amico Dental Care, we believe in complete transparency about complications with implants and all aspects of dental implant treatment. While implants have a 95% success rate, it’s essential to understand both temporary effects and long-term considerations:
Short-Term Effects (1-2 Weeks Post-Surgery):
✔ Common & Temporary: Swelling (80% of patients), mild bleeding (30%), bruising (15%)
✔ Rare but Manageable: Minor dental implant infections (10%, treated with antibiotics)
Long-Term Considerations:
✔ Preventable dental implant risks: Peri-implantitis (10-20%) and bone loss (5-10%) can be minimized with proper care
✔ Higher Risk Groups: Smokers (3x failure risk) and uncontrolled diabetics (40% higher risk) require special protocols
✔ Temporary Sensitivity: Some patients (3-5%) experience mild pressure/temperature sensitivity that typically resolves within 6 months
Our Proactive Protection Plan:
✓ Pre-Surgical Optimization: Custom protocols for high-risk patients
✓ Precision Placement: Minimally invasive techniques to reduce trauma
✓ Lifetime Maintenance Program: Specialized cleanings and monitoring

D’Amico Dental Care – Where Informed Patients Achieve Lasting Results
How to Minimize the Risk of Complications
Minimizing dental implant risks requires a thorough, multi-phase approach. It begins with a comprehensive pre-operative evaluation, including medical history review, blood tests, and 3D CBCT scans to identify potential risk factors like uncontrolled diabetes or smoking. Studies show that proper blood sugar control in diabetic patients can improve success rates to 89%. The surgical phase demands precision techniques and high-quality materials.
Digital surgical guides boost placement accuracy to 95%, while advanced implant surfaces enhance osseointegration. Post-operative care is equally critical, with antibiotics reducing the risk of infection by 70% and strict oral hygiene cutting the chances of peri-implantitis by 75%.
Long-term success hinges on consistent maintenance and lifestyle adjustments. Patients must commit to professional cleanings every 3-6 months and use specialized implant care tools at home. Smoking cessation is crucial (smokers face 3x higher failure rates), as is avoiding alcohol during healing. Emerging adjuncts, such as probiotic therapy, can further reduce inflammation by 40%. With proper planning, execution, and care, modern implants can achieve 98% osseointegration rates, providing patients with a reliable and long-lasting solution when all protocols are followed diligently. While complications with implants can occur, the combination of our advanced technology and your careful compliance creates optimal conditions for a successful outcome.
| Phase | Key Actions | Impact/Statistics | Critical Factors |
| Pre-Operative Evaluation | |||
| – Medical History | Review systemic conditions (e.g., diabetes, osteoporosis) | Diabetic patients with HbA1c <7%: 89% success rate | Smoking increases failure risk 3x |
| – Diagnostic Imaging | 3D CBCT scans for bone assessment | Identifies nerve proximity/sinus issues | Reduces surgical complications by 60% |
| Surgical Phase | |||
| – Guided Surgery | Use of digital surgical guides | 95% placement accuracy | Avoids vital structures |
| – Implant Surface | Hydrophilic/rough surface implants | Enhances osseointegration speed by 30% | Titanium/zirconia materials are preferred |
| Post-Operative Care | |||
| – Antibiotics | Prophylactic prescription (e.g., amoxicillin) | Reduces infection risk by 70% | Critical for the first 72 hours |
| – Oral Hygiene | Chlorhexidine mouthwash + gentle brushing | Lowers peri-implantitis risk by 75% | Avoid direct implant contact initially |
| Long-Term Maintenance | |||
| – Professional Cleanings | Quarterly cleanings with implant-safe tools | Prevents bone loss (>90% 10-year survival) | Use plastic scalers, not metal |
| – Home Care | Interdental brushes + water flossers | Reduces plaque accumulation by 50% | Avoid abrasive toothpaste |
| – Lifestyle Adjustments | Smoking cessation, limited alcohol during healing | Smokers: 60% success rate vs 95% non-smokers | Probiotics reduce inflammation by 40% |
| Emerging Adjuncts | Probiotic therapy (e.g., L. reuteri) | 40% reduction in inflammatory markers | Supports microbiome balance |
How to Handle Implant-Related Discomfort
Post-operative discomfort after dental implant surgery typically peaks within the first 3-7 days and gradually subsides. Effective pain management includes NSAIDs like ibuprofen (400mg every 6-8 hours for the first 72 hours), which studies show can reduce pain by 60%. Applying cold compresses (20 minutes on/20 minutes off) during the first 24 hours, followed by warm compresses after 48 hours, helps minimize swelling and discomfort. For more severe pain, dentists may prescribe more potent analgesics like acetaminophen with codeine.
Persistent discomfort lasting more than two weeks requires professional evaluation, as it may indicate complications such as dental implant infections, improper implant loading, or tissue reactions. In such cases, treatment may involve adjusting the prosthesis, administering antibiotics, or, in rare instances, removing the implant. Meticulous oral hygiene, avoiding pressure on the implant site, and regular dental check-ups can prevent most long-term issues. Research indicates that patients who strictly follow post-operative instructions experience 75% fewer prolonged discomfort episodes, highlighting the importance of adherence to care protocols for optimal recovery and implant success.

What to Do if Your Implant Fails?
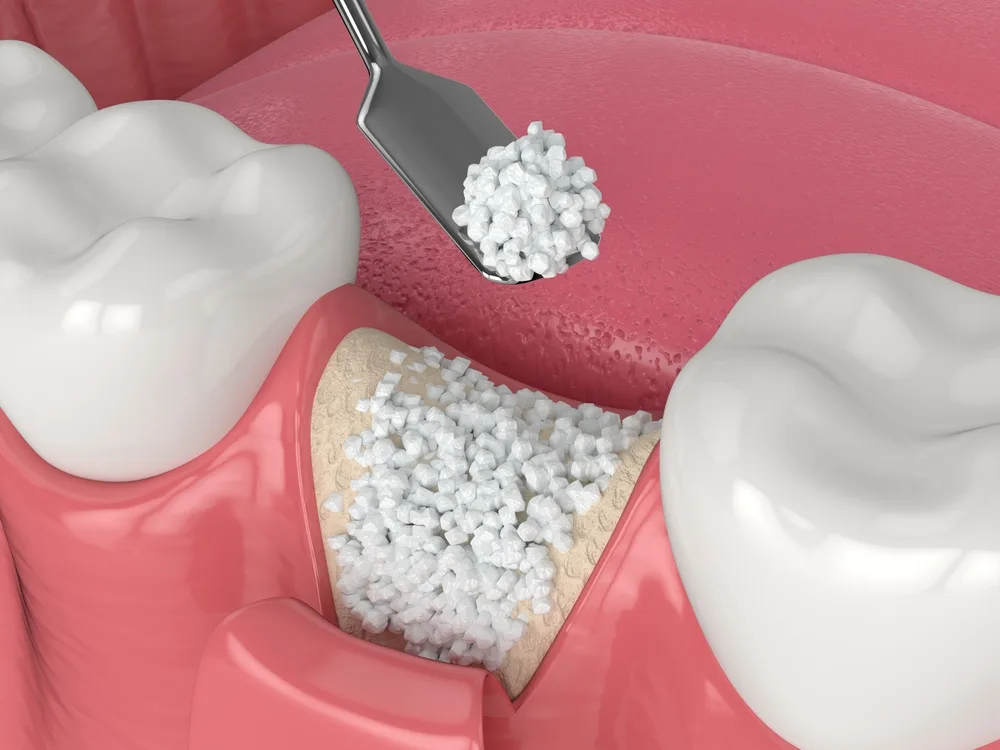
Dental implant failure is an uncommon but manageable occurrence that typically manifests in two forms: acute (pre-loading) and chronic (post-loading). In cases of acute failure, which typically occur within the first six months, dentists conduct thorough clinical and radiographic evaluations to identify the root cause. The most common reasons include infection (43% of cases), inability to withstand functional forces (31%), and osseointegration issues (26%). The initial treatment involves removing the failed implant and, if necessary, performing bone grafting. Research indicates that after 8-12 weeks of healing, replacement implants can be successfully placed with an 85-90% success rate.
Chronic failure, typically caused by advanced peri-implantitis, requires a more complex treatment protocol. Following implant removal, the area undergoes complete debridement, and advanced techniques, such as guided bone regeneration (GBR) or the use of growth factors, are employed. Clinical studies show that combining topical and systemic antibiotics can increase the success rate of replacement implants by up to 35%. When managing dental implant risks, identifying and addressing root causes—whether diabetes control, smoking cessation, or occlusal adjustments—is critical to prevent recurrence. This systematic approach ensures optimal outcomes, even in the most complex cases.
Preventive Measures to Ensure Implant Success
At D’Amico Dental Care, we implement a scientifically validated approach to maximize your implant’s longevity through meticulous pre- and post-operative care:
Pre-Surgical Optimization:
✓ Advanced 3D CT Scans (94% accuracy for bone assessment)
✓ Systemic Health Management: HbA1c <7% for diabetics, smoking cessation (4+ weeks pre-op)
✓ Periodontal Health Preparation to ensure optimal healing conditions
✓ Custom Risk Reduction Plans boosting success rates by 30%
Post-Surgical Excellence:
✓ Specialized Cleaning Protocol: Implant-specific brushes/floss + professional cleanings every 4-6 months
✓ Infection Prevention: Medicated 0.12% chlorhexidine rinses (40% risk reduction)
✓ Occlusal Monitoring: Bite force analysis and prosthesis adjustments
✓ Lifestyle Guidance: Protecting your investment from damaging habits
Our dual-phase protective system combines:
• Preventive Diagnostics with digital planning
• Precision Maintenance through our Implant Longevity Program

Managing Pain and Swelling After Surgery
Acute Phase (0-72 hours):
• Cold Therapy: 20-minute ice pack applications hourly reduce swelling by 40%
• Medication Protocol:
- Ibuprofen 400mg every 6 hours (optimal for pain/inflammation)
- Acetaminophen-codeine for breakthrough pain (dentist-supervised)
• Positioning: 45° head elevation with two pillows decreases swelling 25%
Transition Phase (Day 3+):
• Warm Compresses: Promote circulation for the resolution of residual swelling
• Saltwater Rinses: ½ tsp salt in warm water every 8 hours enhances healing
• Jaw Mobility: Gentle opening/closing exercises from day 3 improve function
Critical Precautions:
→ Activity Restrictions: Avoid strenuous exercise for 7 days
→ Tobacco Cessation: Absolute avoidance for 2 weeks minimum
→ Warning Signs:
- Severe pain persisting >5 days
- Swelling increases after 72 hours
- Requires immediate dental evaluation
Infections and How to Avoid Them
Peri-implantitis is one of the most serious dental implant risks after surgery, affecting 10-15% of cases. If left untreated, it can lead to implant failure. Watch for warning signs, such as increasing swelling, throbbing pain, pus discharge, and an unpleasant odor. Research shows that preventive antibiotics (like amoxicillin + clavulanic acid taken 1 hour before surgery) can reduce infection risk by 70%. Using 0.12% chlorhexidine mouthwash twice daily for 2 weeks after surgery also plays a key role in prevention.
While dental implant risks are low, we take extra precautions, including sterile techniques, protecting the surgical site, and managing health factors such as diabetes, to provide you with the safest possible experience. Studies confirm that smokers have a 3 times higher risk of infection, so quitting at least 4 weeks before and after surgery is crucial. If infection occurs, treatment involves professional cleaning, antibiotics (usually metronidazole + amoxicillin for 7 days), and laser therapy in advanced cases. Regular 6-month checkups are crucial for detecting subclinical peri-implantitis early, before it progresses.
When to Contact Your Dentist After Surgery
At D’Amico Dental Care, we want you to feel confident about your recovery after implant surgery. Here’s what to expect and when to contact us:
Typical Symptoms (First 24-48 Hours):
✔ Mild bleeding/oozing
✔ Localized swelling (peaks at 48 hours)
✔ Moderate discomfort
Red Flags Requiring Immediate Attention:
Bleeding that continues after 30 minutes of firm gauze pressure
Swelling that worsens after day 3 or spreads
Fever above 38°C (100.4°F)
Severe pain unrelieved by prescribed medication
Pus discharge or foul taste/smell
Later Warning Signs (Beyond First Week):
→ Implant mobility (even slight movement)
→ Persistent numbness (lasting >8 hours)
→ Gum recession around the implant
Why Timely Action Matters:
Early intervention for complications like peri-implantitis increases treatment success to 85%. That’s why we emphasize:
✓ Keeping all follow-up appointments (1 week, 1 month, 3 months)
✓ Reporting any concerns immediately – no question is too small
Psychological Impact of Dental Implant Complications
Dental implant complications can have significant emotional consequences for patients. Studies show that approximately 35% of patients who experience implant failure report noticeable anxiety and reduced self-confidence. This effect is particularly pronounced in individuals with pre-existing mental health concerns or those who have invested substantial financial resources in their treatment. Research published in the Journal of Oral Rehabilitation (2022) found that patients facing implant complications were 2.5 times more likely to experience symptoms of depression compared to others.
Psychological support can make a meaningful difference. Clear communication about potential dental implant risks before surgery, discussing alternative treatment options, and providing emotional support after complications arise are all effective strategies for ensuring patient well-being. Counseling sessions with the dentist—and referral to a psychologist when needed—can help patients adjust to their situation. Studies indicate that patients who receive this type of support adapt emotionally 40% faster. If you’re feeling anxious or discouraged after an implant complication, remember—you’re not alone, and help is available.
source: www.webmd.com
FAQ
- What immediate side effects might occur?
✓ Swelling/bruising (normal for 3-5 days)
✓ Mild-moderate pain (manageable with medication)
✓ Minor bleeding (first 24 hours)
✓ Temporary numbness (rare nerve proximity cases)
✓ Local infection (if hygiene isn’t maintained)
- What issues may develop months later?
✓ Peri-implantitis (bone loss around the implant)
✓ Implant loosening/failure
✓ Implant rejection (rare)
✓ Sinus issues (upper jaw implants)
✓ Gum inflammation around the implant
- Who faces higher complication risks?
- Smokers (3× higher failure risk)
• Uncontrolled diabetics
• Autoimmune disease patients
• Bisphosphonate therapy recipients
• Those with poor oral hygiene
- How serious is peri-implantitis?
- Inflammatory disease similar to periodontitis
- Symptoms: Red/swollen gums, bleeding, bone loss
- Leads to implant loss if untreated
- 10-15% occurrence after 5-10 years
- Preventable with proper care and checkups
- Why do some implants fail?
✓ Failed osseointegration
✓ Premature overloading
✓ Bacterial infection
✓ Surgical technique errors
✓ Poor bone quality
- How can upper jaw implants affect the sinuses?
✓ Rare sinus cavity penetration
✓ Post-op sinusitis
✓ Need for sinus lifts (insufficient bone)
✓ Symptoms: Sinus pressure, nasal discharge
✓ Typically treatable with antibiotics
- Can implants damage nerves?
✓ Lower jaw: Risk to the inferior alveolar nerve
✓ Symptoms: Persistent lip/chin numbness
✓ Usually temporary (weeks to months)
✓ Rarely permanent
✓ Preventable with CT planning
- How to minimize complications?
✓ Choose an experienced implantologist
✓ Complete all pre-op evaluations
✓ Quit smoking (2+ weeks pre/post-op)
✓ Control systemic conditions like diabetes
✓ Strictly follow post-op instructions