Bone grafting for dental implants is a crucial procedure for patients who lack sufficient bone volume or density to support dental implants, often necessary after severe bone loss resulting from tooth extraction or advanced periodontal disease.
The healing process typically takes 4-9 months, depending on the graft type and the size of the treatment area, during which new bone forms to support future implants. Advanced techniques, such as sinus lifts for the upper jaw or ridge augmentation for the lower jaw, can achieve remarkable results. Emerging research shows platelet-rich fibrin (PRF) can accelerate healing by up to 30%.
This blog is specially designed for you, whether you’re considering dental implant treatment or want to learn more about bone grafting for dental implants. Here, we’ll cover:
✓ Everything about bone grafting for implants – its benefits, potential risks, and what to expect
✓ Answers to all your questions about the implant process from start to finish
✓ Expert insights to help you make informed decisions about your dental health
Why Bone Grafting For Dental implants is Necessary for Some Patients?
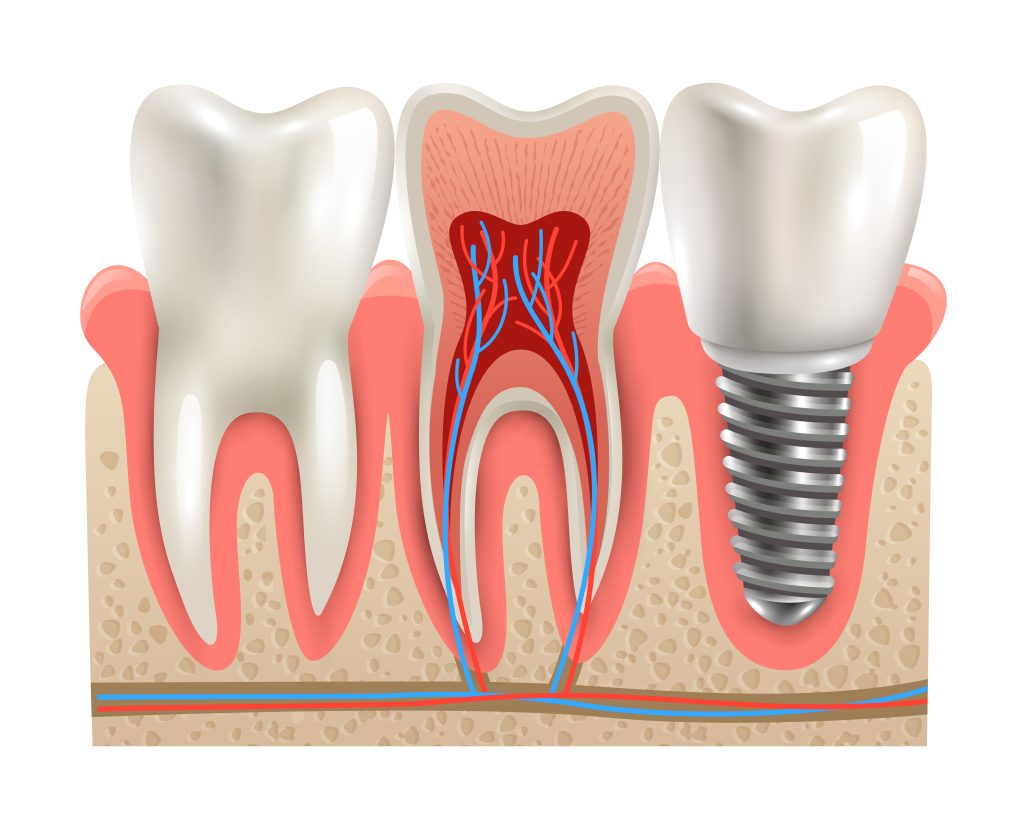
At D’Amico Dental Care, we recognise bone grafting as an essential procedure for patients with jawbone loss due to missing teeth, periodontal disease, or injury. When bone dimensions shrink below the critical thresholds of 10mm height or 5mm width, grafting becomes necessary to create a stable foundation for implants. Our preferred method utilises your bone (autograft), harvested from the chin or jaw, which offers exceptional success rates of 95-98% and can help your implants last over 20 years. Beyond functional benefits, grafting preserves your facial structure by preventing the sunken appearance that often accompanies bone loss, particularly in visible smile areas.
We employ cutting-edge techniques at D’Amico Dental Care, including platelet-rich fibrin (PRF) to accelerate healing and 3D imaging for precise graft placement. While it requires an additional procedure, bone grafting transforms marginal cases into outstanding, long-term successes by rebuilding the natural architecture of your jaw. This investment in your oral foundation pays lifelong dividends, ensuring both the performance and aesthetics of your future restoration. During your consultation, we’ll explore whether simultaneous grafting can optimise your treatment timeline while delivering the exceptional results you deserve.
The Bone grafting for dental implants Procedure
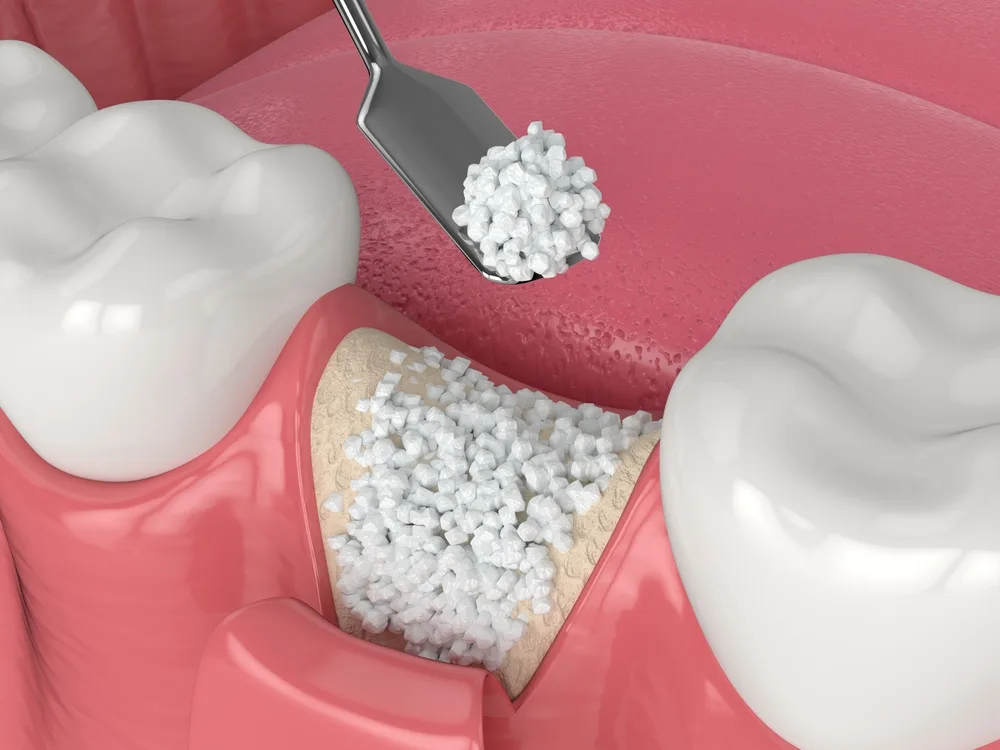
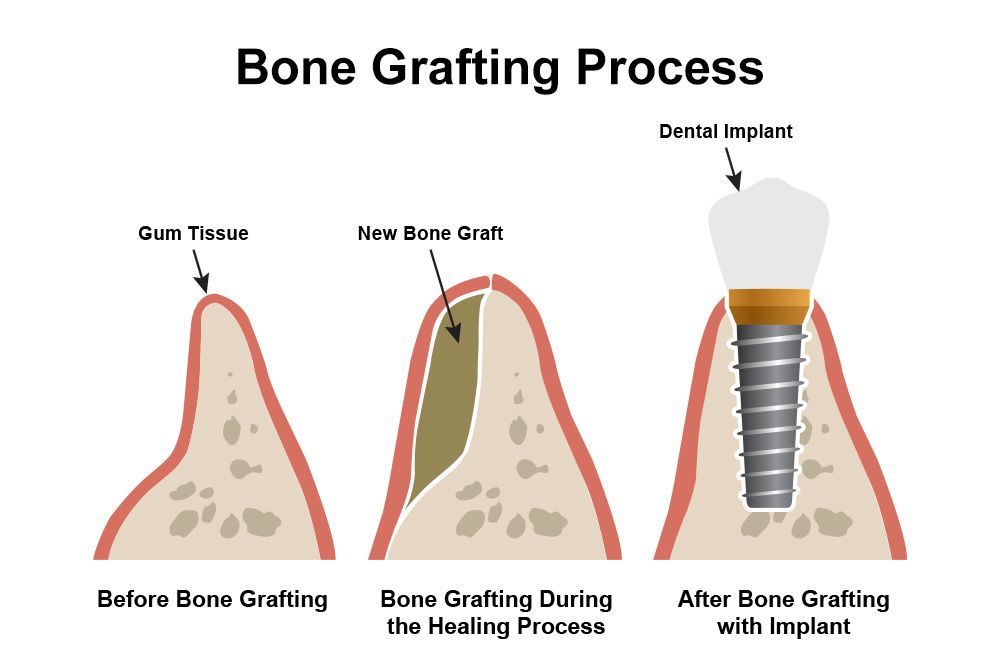
Bone grafting for dental implants is a specialised surgical technique performed in three key stages. First, the recipient site (future implant location) is prepared by creating a gingival flap. The grafting material, which may be autograft (patient’s bone from chin or ramus), allograft (processed human bone), or synthetic substitutes, is then carefully placed. Studies demonstrate that the use of regenerative membranes prevents unwanted cell migration in 85% of cases, thereby protecting the grafted area.
The 4-9 month healing phase follows, during which new bone forms. Patients must maintain a soft diet and meticulous oral hygiene throughout this period. Research confirms that platelet-rich plasma (PRP) can accelerate healing by 30%. Once bone integration is confirmed through imaging, the implant is placed in its optimal position. Advanced techniques, such as sinus lifts for the upper jaw or ridge reconstruction for the lower jaw, are tailored to each patient’s unique anatomy. Success rates of 90-95% in specialised centres depend on surgical skill, graft material selection, and patient compliance with postoperative care.
Types of Bone Grafts Used in Implant Surgery
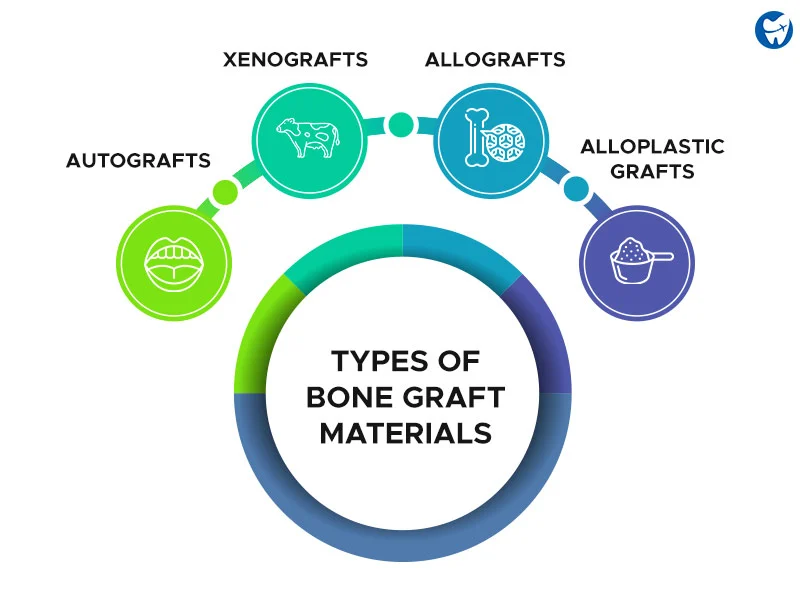
Dental implant procedures utilise four primary bone graft types, each with unique advantages and limitations:
- Autograft (Gold Standard): Uses the patient’s bone, typically harvested from the chin, jaw ramus, or hip. This method boasts a 95-98% success rate due to its use of living cells and natural growth factors, although it requires a second surgical site for bone extraction.
- Allograft: Utilises processed and sterilised human donor bone from tissue banks. With minimal rejection risk and an 85-90% success rate, it eliminates the need for a second surgery while providing excellent results.
- Xenograft: Derived from animal sources (usually bovine or porcine), these grafts retain only the mineral bone matrix after processing. They slowly resorb while serving as a scaffold for new bone growth.
- Alloplast: Synthetic materials, such as hydroxyapatite or tricalcium phosphate, offer complete biocompatibility. Often combined with biological agents, they enhance osteoconductive properties for effective bone regeneration.
Selection Factors: The optimal graft depends on the severity of bone loss, the anatomical location, and the surgeon’s preference. Current research shows that combining these materials with growth factors (e.g., BMP-2) can significantly enhance outcomes. Modern techniques increasingly blend multiple graft types to maximise benefits while minimising drawbacks.
Recovery Time After Bone grafting for dental implants
The healing timeline after bone grafting for dental implants depends on the complexity of the procedure and your biological response. Minor grafts (like socket preservation) typically heal in 2-4 weeks, while major reconstructions (such as sinus lifts) may require 6-12 months for full integration.
At D’Amico Dental Care, we use advanced techniques like PRP/PRF growth factors to accelerate healing by 30%, though smoking can drastically delay recovery by 50% and triple failure risks. The first 72 hours are critical; strictly follow our protocol, which includes cold compresses, prescribed antibiotics, and rest. For the next 4-8 weeks, maintain a soft diet and avoid pressure on the grafted area to protect the delicate new bone formation.
After 3-4 months, we’ll use 3D imaging to assess bone integration before proceeding with implant placement. Studies confirm that patients who adhere to post-operative instructions achieve a 95% success rate, making your commitment to recovery just as vital as our surgical precision. While healing times vary, this foundational phase ensures your implant will have the strongest, most stable base for long-term success. At D’Amico Dental Care, we closely monitor your progress and tailor recommendations to your unique healing response, ensuring optimal results for your future smile.

The Impact of Bone Grafting on Implant Success
Bone grafting has emerged as a critical factor in enhancing dental implant success rates, particularly for patients with significant bone loss. Long-term studies have demonstrated that proper bone grafting can significantly improve implant success rates, increasing from 65% to 95% in patients with bone deficiency, by creating an ideal foundation for osseointegration. Autografts (using the patient’s bone) consistently show the highest success rates due to their natural growth factors.
Beyond mechanical stability, bone grafting for dental implants provides significant aesthetic benefits, particularly in the anterior jaw region, where it prevents soft tissue collapse and facial deformities. Advanced techniques, such as short-term sinus lifts and computer-guided ridge reconstruction, have significantly improved precision; however, outcomes still depend on the quality of the graft, surgical expertise, and patient compliance with postoperative care.
While revolutionary, bone grafting for dental implants presents certain considerations: the process requires an extended healing period (4-9 months), carries a small risk of infection (<5% at specialised centres), and involves higher costs compared to conventional implants. However, for patients with bone loss, these factors are often outweighed by the substantial benefits of restored chewing function, preserved facial aesthetics, and long-term implant stability. Modern techniques continue to mitigate these challenges, making bone grafting an increasingly accessible option for patients who previously might not have been eligible for dental implants. The investment in time and resources frequently translates to decades of improved oral health and quality of life.
Risks and Complications of Bone Grafting for Dental Implants
At D’Amico Dental Care, we prioritise patient safety while achieving exceptional success rates of 85-95% with bone grafting for implant procedures. While generally safe, it’s essential to understand the potential complications, including surgical site infections (3-5% of cases), temporary swelling and pain (which typically resolve within a week), and minor bleeding. Higher-risk patients should note that smoking quadruples infection risks while uncontrolled diabetes triples graft rejection rates. For sinus lifts specifically, 10-15% of cases may involve minor sinus membrane perforations, though our surgeons are trained to repair these during your procedure immediately.
Though rare (1-2% of cases), more serious concerns like nerve irritation or graft rejection can be reduced by 70% through our advanced protocols:
✓ Microscopic surgical techniques for precision
✓ Growth factor enhancements (PRP/PRF)
✓ Customised healing plans for high-risk patients
Your commitment to post-op instructions (especially smoking cessation and medication adherence) plays an equally vital role in minimising risks. Most importantly, choosing an experienced specialist at a well-equipped facility like D’Amico Dental Care dramatically improves outcomes through:
→ CBCT-guided planning
→ Sterile surgical protocols
→ 24/7 emergency support
source: www.guysandstthomas.nhs.uk
FAQ
- Why might dental implants require bone grafting?
- Jawbone resorption after tooth extraction (up to 40% in the first year)
- Insufficient bone volume for implant stability
- Prevention of aesthetic complications like facial collapse
- Better distribution of chewing forces on implants
- Increased success rate up to 95%
- What bone graft materials are used for implants?
- Autograft: Patient’s bone (from chin or hip)
- Allograft: Processed human donor bone
- Xenograft: Animal-derived (typically bovine)
- Synthetic materials: Hydroxyapatite or tricalcium phosphate
- PRF: Platelet-rich fibrin from the patient’s blood
- How is bone grafting for dental implants performed?
- Local or general anaesthesia
- Gum flap elevation and site preparation
- Graft material placement in the target area
- Protective membrane coverage (when needed)
- Suturing with a 3-6 month healing period
- Are grafting and implant placement simultaneous?
- Staged approach: For severe deficiencies (4-6 months prior)
- Simultaneous: With minor bone deficiencies
- Sinus lift: Typically 6-9 months before upper jaw implants
- Block grafts: Require extended healing time
- What care is needed after bone grafting?
- Prescribed antibiotics and analgesics
- Soft diet for 2-4 weeks
- Avoid strenuous activity for 1 week
- No smoking for a minimum of 4 weeks
- Gentle saltwater rinses after 24 hours
- Does bone grafting for dental implants have risks?
- Swelling/bruising (normal for 3-5 days)
- Mild-moderate pain (controlled with medication)
- Minor bleeding within the first 24 hours
- Infection (if hygiene is neglected)
- Graft rejection (rare, <5% cases)
- How does grafting improve implant success?
- Success increased from 60% to 90-95%
- Bone quality improvement in 85-90% of cases
- Long-term implant stability
- Superior aesthetic gumline results
- Optimal force distribution when chewing
- What are the costs and insurance coverage?
- Basic grafting: 1.5-4 million Tomans
- Sinus lift: 3-6 million Tomans
- Block grafts: 5-8 million Tomans
- Insurance coverage: Typically limited/excluded
- Long-term savings: Reduces implant replacement needs